AI is reshaping spine health care by delivering faster, more accurate, and consistent results compared to manual methods. Traditional approaches, like manual imaging analysis and data entry, often lead to delays and variability due to human factors such as fatigue and experience. Meanwhile, AI-powered tools process complex data instantly, identify patterns in medical imaging, and predict patient outcomes with high precision.
Key takeaways:
- Speed: AI systems analyze imaging data up to 78% faster than manual methods.
- Accuracy: AI achieves superior precision in diagnosing conditions like scoliosis and spinal stenosis.
- Predictive Power: AI models forecast recovery outcomes and risks using multimodal data, surpassing static traditional metrics.
- Workflow Efficiency: AI automates tasks like data entry and monitoring, reducing delays in diagnosis and care.
AI-driven devices, such as wearables, also provide real-time spine health monitoring, offering immediate feedback and personalized care plans. While challenges like data privacy and bias remain, AI is transforming spine health care by improving diagnostic accuracy, streamlining workflows, and enabling earlier interventions.
How AI Is Revolutionizing Spine Surgery
sbb-itb-44aa802
Accuracy and Detection Performance
AI vs Traditional Methods in Spine Health Analysis: Speed, Accuracy and Workflow Comparison
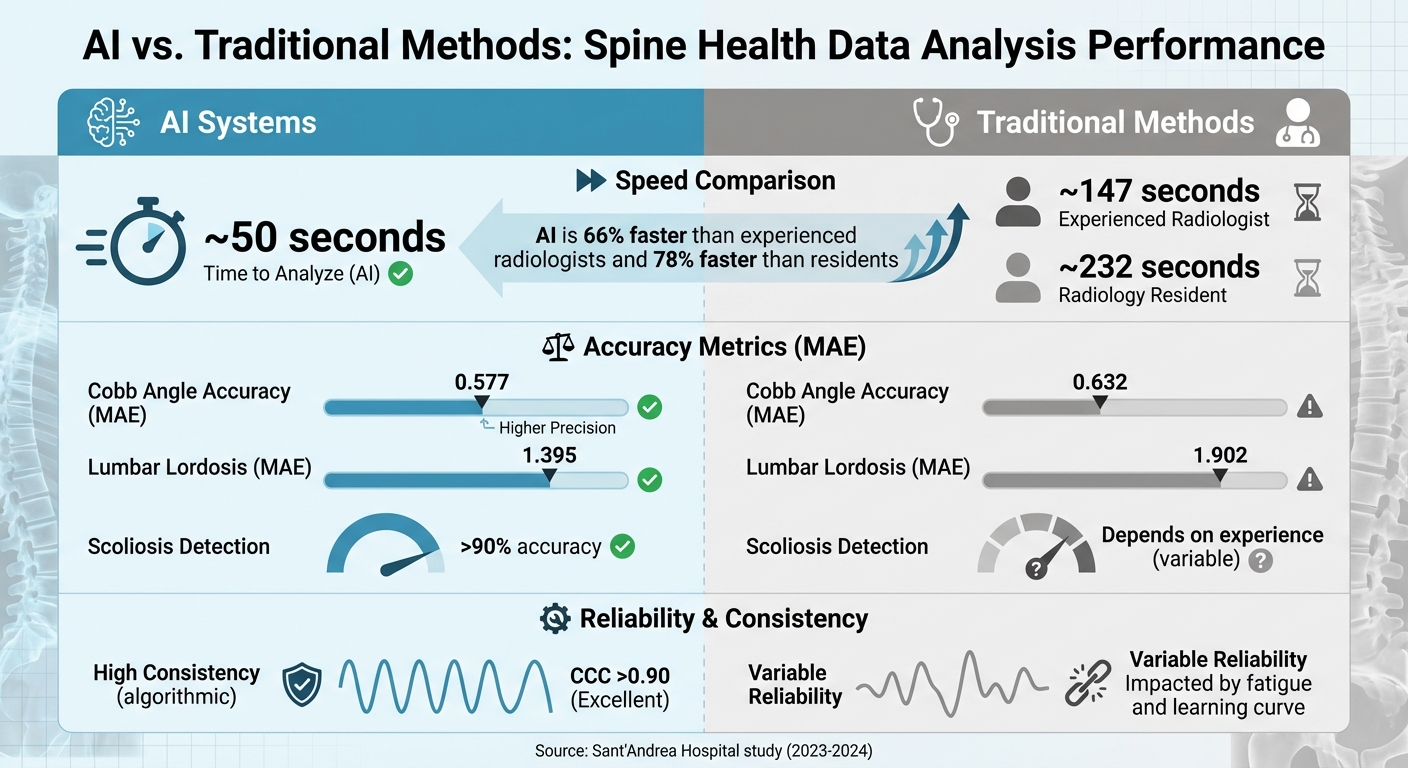
To understand AI’s role in spine health, let’s break down how it compares to traditional methods in terms of accuracy, speed, and consistency.
How AI Detection Systems Work
AI-powered systems leverage advanced algorithms, such as CNNs and U-Net architectures, to automatically pinpoint anatomical landmarks and measure spinal parameters from X-rays and MRIs. These tools can identify conditions like scoliosis, fractures, and spinal stenosis with remarkable precision.
For example, between January 2023 and October 2024, researchers at Sant’Andrea Hospital (Sapienza University of Rome) tested BoneMetrics (version 2.3.1 by Gleamer) on 56 patients. The AI achieved a Concordance Correlation Coefficient (CCC) greater than 0.9, demonstrating excellent alignment with human experts. Its Mean Absolute Error (MAE) for Cobb angle measurements was 0.577, outperforming a radiology resident’s MAE of 0.632.
Another example is AIH LLC‘s aiSpine, which uses similar AI-driven methods for real-time posture monitoring. This device detects spinal misalignment and provides immediate feedback, such as vibration alerts, making it useful even outside clinical environments.
In contrast, traditional diagnostic methods rely on manual processes, which can be time-consuming and prone to variability.
How Traditional Diagnosis Works
Conventional spine diagnosis involves radiologists manually interpreting imaging scans, such as X-rays, MRIs, and CTs. They visually identify landmarks and measure angles using digital tools, relying heavily on their expertise and experience. This process typically takes 147 seconds for an experienced radiologist and 232 seconds for a resident per case.
However, manual diagnosis introduces variability. Practitioners may interpret landmarks differently, leading to inconsistent measurements. Factors like fatigue, distractions, and differing skill levels further affect accuracy. A 2025 study from Osaka Metropolitan University found that nine experienced spine surgeons achieved only 60.6% average accuracy when diagnosing osteopenia and osteoporosis from cervical radiographs.
These challenges highlight the limitations of traditional methods, particularly in terms of time and reliability.
Comparison Table: Accuracy, Speed, and Reliability
| Metric | AI Systems (e.g., BoneMetrics) | Experienced Radiologist | Radiology Resident |
|---|---|---|---|
| Analysis Time | ~50 seconds | ~147 seconds | ~232 seconds |
| Cobb Angle Accuracy (MAE) | 0.577 | Reference Standard | 0.632 |
| Lumbar Lordosis (MAE) | 1.395 | Reference Standard | 1.902 |
| Reliability (CCC) | >0.90 (Excellent) | Variable | Variable |
| Consistency | High (Algorithmic) | Impacted by fatigue | Impacted by learning curve |
| Scoliosis Detection | >90% accuracy | Depends on experience | Depends on experience |
AI systems stand out by delivering results 66% faster than experienced radiologists and 78% faster than residents, all while maintaining consistent precision across measurements. Unlike manual methods, AI eliminates variability caused by human factors like fatigue or workload, ensuring reliable results every time.
Data Processing Speed and Workflow
Speed is everything when it comes to spine care. Think about it: when a patient arrives at a clinic with spine pain, every extra minute spent on manual tasks like entering data, reviewing charts, or making calculations slows down their path to diagnosis and treatment. AI changes the game by handling these tasks instantly, while traditional methods still rely on time-draining processes.
Real-Time Analysis with AI
AI-powered tools analyze spine health data the second it’s collected. Take wearable devices like AIH LLC’s aiSpine, for example. These devices monitor posture continuously, detect spinal misalignment, and send instant vibration alerts. This immediate feedback eliminates the weeks-long gap between clinic visits that often comes with traditional monitoring approaches.
Digital platforms now sync with wearables to deliver personalized, real-time recommendations. These systems run 24/7, processing data and generating tailored advice in mere seconds – no human input required.
"AI’s unique capacity to integrate vast and complex data, learn from patterns, and generate predictive insights, positions it as an invaluable tool for optimizing clinical workflows."
– Victoria A Bensel, DC, MS, MPH
In surgical settings, AI-enabled robotic systems and augmented reality (AR) provide real-time 3D visualizations during procedures. This technology ensures sub-millimeter precision in instrument placement, eliminating the delays of manual estimations. Meanwhile, deep learning reconstruction (DLR) has drastically enhanced the speed and clarity of MRI and CT imaging compared to older, non-AI methods.
Traditional workflows simply can’t compete with this level of efficiency and speed.
Time Requirements in Traditional Workflows
Traditional methods are weighed down by manual processes. Take electronic health records (EHR) as an example: entering data manually is so time-intensive that thousands of medical scribes are employed just to manage documentation. Even then, 72% of office-based physicians report that documentation burdens impact their practice.
Chart reviews also take time, delaying decisions. AI, on the other hand, can instantly access vast networks of over 200 billion patient records. This stark difference highlights how outdated methods slow down care.
Imaging analysis is another bottleneck. Manual measurements take time, and when you multiply that by the number of daily cases, the delays add up quickly. These inefficiencies can push back treatment timelines significantly.
Comparison Table: Processing Time and Workflow Effects
| Workflow Element | Traditional Methods | AI-Driven Systems |
|---|---|---|
| Data Entry | Manual EHR entry | Ambient voice-to-EMR transcription |
| Patient Assessment | Manual review of symptoms and history | Autonomous triage bots (91.7% accuracy) |
| Imaging Analysis | Manual measurement | Automated segmentation with faster processing |
| Patient Monitoring | Periodic clinic visits; delayed reports | Real-time tracking via wearables and apps |
| Reporting Speed | Days to weeks for reports | Instant analysis and feedback |
| Workflow Integration | Fragmented; resource-heavy | Continuous monitoring with automation |
Traditional workflows break care into separate steps – office visits, imaging appointments, follow-ups – each requiring its own scheduling and coordination. AI flips this model on its head, creating a seamless flow of data from wearables to digital platforms and straight to providers. This continuous care model has fueled a surge in AI-related research in spine surgery, with over 300 publications annually by 2024.
This shift doesn’t just save time; it enables earlier diagnoses and better spine health management by making clinical interventions faster and more effective.
Prediction and Personalized Analysis
AI isn’t just about analyzing what’s happening now – it’s about looking ahead. When it comes to predicting patient outcomes, AI takes a clear lead. Traditional methods, like measuring Cobb angles on X-rays or assessing disc heights on MRIs, provide a snapshot of a patient’s current condition. But they often fall short when it comes to forecasting future health or tailoring care. AI, on the other hand, digs deep into massive datasets to predict outcomes, flag potential risks early, and craft treatment plans tailored to the individual. This real-time, forward-thinking approach is reshaping spine care.
What AI Can Predict
AI combines imaging, clinical history, and even genetic data to predict outcomes that go far beyond standard radiographic measures. Take, for example, a 2024 study conducted at Shriners Children’s hospitals in Greenville and Lexington. Researchers examined 455 pediatric scoliosis patients, using 171 pre-operative clinical features. Their machine-learning models achieved impressive accuracy in predicting post-operative quality-of-life outcomes: an AUROC of 0.86 at six months, 0.85 at one year, and 0.83 at two years. These models also pinpointed which patients were likely to reach the "Minimum Clinically Important Difference" (MCID) – the point where patients genuinely feel better. In contrast, traditional radiographic correction rates, which typically range from 60% to 80%, have consistently failed to predict patient satisfaction effectively.
"AI leverages integrated datasets to tailor predictions and optimize care, supporting personalized treatment strategies."
– Victoria A. Bensel, DC, MS, MPH, Yale University
AI techniques like radiomics can extract subtle image features that are critical for assessing risks, such as adjacent-level fractures after vertebroplasty. It also facilitates personalized care through tools like wearables – think of devices like aiSpine – that adjust treatment plans in real time, creating a care model that’s as unique as the patient.
While AI provides a glimpse into the future, traditional methods remain stuck in the present, as outlined below.
Constraints of Traditional Analysis
Traditional methods rely on static measurements, offering limited insight into what lies ahead. Fixed scoring systems and radiographic metrics dominate spine health analysis, but research shows no strong link between these metrics and patient-reported outcomes. For instance, even an 80% improvement in Cobb angle doesn’t necessarily mean a better quality of life for the patient.
Traditional clinical prediction models, often based on logistic regression, also have their limits. They depend on manually selected predictors, which restrict the number of variables they can handle. This approach struggles to account for the complex, nonlinear relationships found in patient data, leading to a one-size-fits-all approach that ignores individual factors like genetics, demographics, and functional status.
Comparison Table: Prediction Accuracy and Customization
| Feature | Traditional Static Analysis | AI Prediction Models |
|---|---|---|
| Data Input | Radiographic only (e.g., Cobb angles, MRI) | Multimodal (imaging, clinical, genetic, wearables) |
| Adaptability | Fixed scoring systems; manual descriptors | Learns patterns; adapts to individual differences |
| Outcome Focus | Static radiographic results | Subjective outcomes, MCID, long-term recovery |
| Prediction Accuracy | Inconsistent; weak link to patient satisfaction | High (AUROC 0.83–0.86 for long-term outcomes) |
| Variable Handling | Limited; manual selection | Automatic processing of over 170 features |
| Clinical Utility | Standardized benchmarks | Enables shared decision-making and personalized guidance |
AI is driving a shift from reactive care to proactive management. Tools like polygenic risk scores and genome-wide association studies (GWAS) are now identifying at-risk patients before symptoms even appear. Combined with continuous monitoring, this approach creates a personalized care model that evolves with the patient’s recovery journey – something traditional methods simply can’t match.
Conclusion: What’s Next for Spine Health Data Analysis
Why AI Works Better for Spine Health
AI has proven to outperform traditional methods in spine health analysis, offering greater accuracy, faster results, and stronger predictive capabilities. For instance, AI systems now rival or surpass radiologists in identifying vertebral fractures and disc herniations. Unlike the slower, batch-based workflows of the past, AI enables real-time data processing, which is a game-changer for spine care. By integrating imaging data, clinical histories, and genetic markers, AI provides highly precise outcome predictions.
Consider these advancements: AI-driven surgical planning has slashed complication rates from 22% to just 4.7%. Meanwhile, automated biomechanical modeling has reduced the time needed to prepare spine models by a staggering 97.9% – shrinking the process from over 24 hours to just about 31 minutes. Of course, challenges like data privacy, algorithmic bias, and explainability still need attention.
"AI and ML promise significant improvements in diagnostic accuracy, treatment personalization, service accessibility, and cost efficiency, paving the way for more streamlined and effective spine care."
– Aqil M Jawed, Department of Orthopaedic Surgery, Shengjing Hospital
These advancements highlight how AI tools are reshaping the landscape of spine care, making it more efficient and precise than ever before.
Using New Technology for Better Results
Taking these AI advantages a step further, advanced wearables are already delivering real-world benefits. Devices like AIH LLC’s aiSpine and aiRing showcase how AI-powered tools are transforming spine monitoring. The aiSpine device, for example, offers real-time posture tracking, vibration reminders, and historical data analysis, enabling tailored therapy plans. Meanwhile, the aiRing – a waterproof health monitoring ring – tracks vital signs through intelligent sensors, seamlessly syncing with the AIH Health App for a comprehensive view of patient health.
Far from replacing clinicians, these technologies enhance clinical decision-making. AI acts as a virtual assistant, offering probabilistic insights and decision support throughout the care journey – from initial assessments to rehabilitation. Wearables also enable remote therapeutic monitoring, allowing early detection of disease recurrence. By combining data from multiple sources, AI can even identify at-risk patients before symptoms develop. This shift from reactive to proactive care is no longer a distant goal; it’s already happening, and the tools to make it a reality are within reach.
FAQs
How does AI enhance spine health diagnosis compared to traditional methods?
AI is transforming spine health diagnosis by using advanced algorithms to examine medical images with high accuracy. It can detect, categorize, and pinpoint radiological findings more effectively than conventional methods, significantly lowering the chances of misdiagnosis.
Beyond diagnostics, AI offers predictive insights into possible clinical outcomes, helping doctors create more tailored and effective treatment plans. This blend of accuracy and forward-looking analysis positions AI as a valuable asset in advancing spine health care.
What challenges does AI face in improving spine health care?
AI holds the promise of reshaping spine health care, but it’s not without its hurdles. A major concern lies in the quality of data used to train AI models. Spinal disorders are highly intricate, and inconsistencies in imaging data can make it tough to develop algorithms that are both dependable and broadly applicable. On top of that, AI tools need to pass rigorous testing and validation processes to ensure they meet strict safety and performance standards.
Another significant challenge is seamlessly integrating AI into clinical workflows. This means tackling issues like making AI systems more interpretable, reducing bias in training data, and adhering to complex healthcare regulations. Privacy concerns and the demand for large, high-quality datasets further complicate the process. While the potential of AI in spine care is immense, addressing these obstacles is critical to fully realizing its impact.
How do AI-powered wearables help with monitoring spine health in real time?
AI-powered wearables bring a new level of convenience to spine health monitoring by keeping tabs on posture, movement, and other essential factors in real time. These gadgets process data on the spot, delivering tailored feedback and spotting potential problems early.
By shedding light on daily habits and patterns related to spine health, these devices empower users to take proactive steps and make smarter choices to boost their overall well-being.

