Wearable health devices are transforming how we monitor and manage our health. These gadgets, ranging from fitness trackers to clinical-grade tools, provide real-time data on vital signs, enabling early detection of issues and better chronic condition management. By collecting up to 1,440 measurements daily, they offer a detailed view of your health compared to traditional spot-checks.
Key Takeaways:
- How They Work: Devices use sensors (optical, electrical, mechanical, biochemical) to track metrics like heart rate, glucose levels, and respiratory patterns. AI processes this data into actionable insights.
- Health Applications: Manage chronic conditions (e.g., diabetes, heart disease), improve sleep, and monitor posture or movement.
- Benefits: Continuous monitoring, early detection, and remote feedback empower users and healthcare providers alike.
- Challenges: Accuracy issues for certain skin tones, data privacy concerns, and usability hurdles like "wearables fatigue."
- Choosing a Device: Look for features aligned with your needs, validated accuracy, and compatibility with your smartphone.
Wearables are tools, not replacements for medical care. They shine when paired with professional guidance, helping you stay informed and proactive about your health.
Healthcare IoT: Wearables & Remote Patient Monitoring Explained | Internet of Things
How Do Wearable Health Devices Work?
Wearable Health Device Sensor Types and Technologies Comparison
Wearable health devices are designed to turn raw physiological data into meaningful health insights, offering a way to monitor your body continuously. These gadgets combine sensors, processors, connectivity, and AI to keep tabs on your health 24/7.
Core Components of Wearable Devices
At the core of every wearable device is a system of sensors that pick up changes in your body. For instance:
- Optical sensors: These use light-emitting diodes (LEDs) and photodetectors to measure blood volume changes through a process called photoplethysmography (PPG). Green LEDs are typically used for heart rate tracking, while red and infrared LEDs are used to measure blood oxygen levels (SpO₂).
- Electrical sensors: These capture biopotentials, like heart rhythms through ECG sensors or stress levels by measuring sweat production with EDA sensors.
- Mechanical sensors: Accelerometers and gyroscopes track movement, steps, and posture. Advanced versions, like seismocardiography (SCG), can even detect chest vibrations caused by heart valve movements.
- Biochemical sensors: Found in devices like continuous glucose monitors (CGMs), these measure glucose levels in interstitial fluid through a sensor placed under the skin. Researchers are also exploring sensors for sweat and saliva biomarkers.
To improve performance, many wearables use flexible materials such as PDMS, Ecoflex, or graphene. These materials conform closely to the body, reducing interference and improving signal clarity. AI and machine learning then analyze the data, detecting conditions like atrial fibrillation or predicting potential heart failure.
"Wearable devices are digital medicine tools that process data captured by mobile sensors to generate measures of behavioral and/or physiological function."
– Andrew Hughes, Vanderbilt University Medical Center
Once the sensors collect information, the real magic happens as the data is processed and interpreted.
Data Flow in Wearable Devices
After gathering raw signals from your body, the device’s processing unit steps in. Using machine learning, it filters out interference – like motion artifacts – and refines the data. This cleaned-up information is then either analyzed directly on the device or sent to a smartphone or cloud server via Bluetooth, Wi‑Fi, or Near Field Communication (NFC).
On your phone or in the cloud, algorithms transform the raw data into actionable insights. These could range from irregular pulse alerts to glucose warnings or even real-time interventions tailored to your condition. Some advanced devices can operate as closed-loop systems, meaning they automatically initiate specific actions based on the data they collect.
Take, for example, the 2019 Apple Heart Study, which involved 419,297 participants. This study tested PPG technology for arrhythmia detection, finding that 0.52% of participants received irregular pulse notifications. Among those who used an ECG patch afterward, the technology had a positive predictive value of 0.84 for detecting atrial fibrillation. Similarly, the Huawei Heart Study, which monitored 187,912 people, identified suspected atrial fibrillation in 0.2% of participants, with a positive predictive value of 91.6%.
While data processing is key, wearable devices also come in various forms to meet different health needs.
Types of Wearable Health Devices
Wearables come in many shapes and sizes, each designed for specific purposes. Some common examples include:
- Smartwatches and fitness trackers: Popular brands like Apple, Samsung, and Fitbit combine heart rate sensors and motion tracking to monitor cardiovascular activity, steps, sleep, and overall physical activity. These devices support both general wellness and chronic condition management.
- Continuous glucose monitors (CGMs): These devices use a sensor placed under the skin to track glucose levels in real time, helping individuals with diabetes manage their condition more effectively.
- ECG patches: Adhesive patches like the Zio Patch are worn on the chest to continuously record heart rhythms over several days, helping detect arrhythmias that might not show up during a brief clinical exam.
- Biosensors and e-textiles: These integrate conductive fibers into clothing to monitor ECG and respiration discreetly over long periods.
- Medical-grade devices: Devices like the BioButton can record up to 1,440 vital sign measurements per day, far surpassing the four manual checks typically done in a hospital. This allows for earlier detection of health changes in patients with chronic conditions.
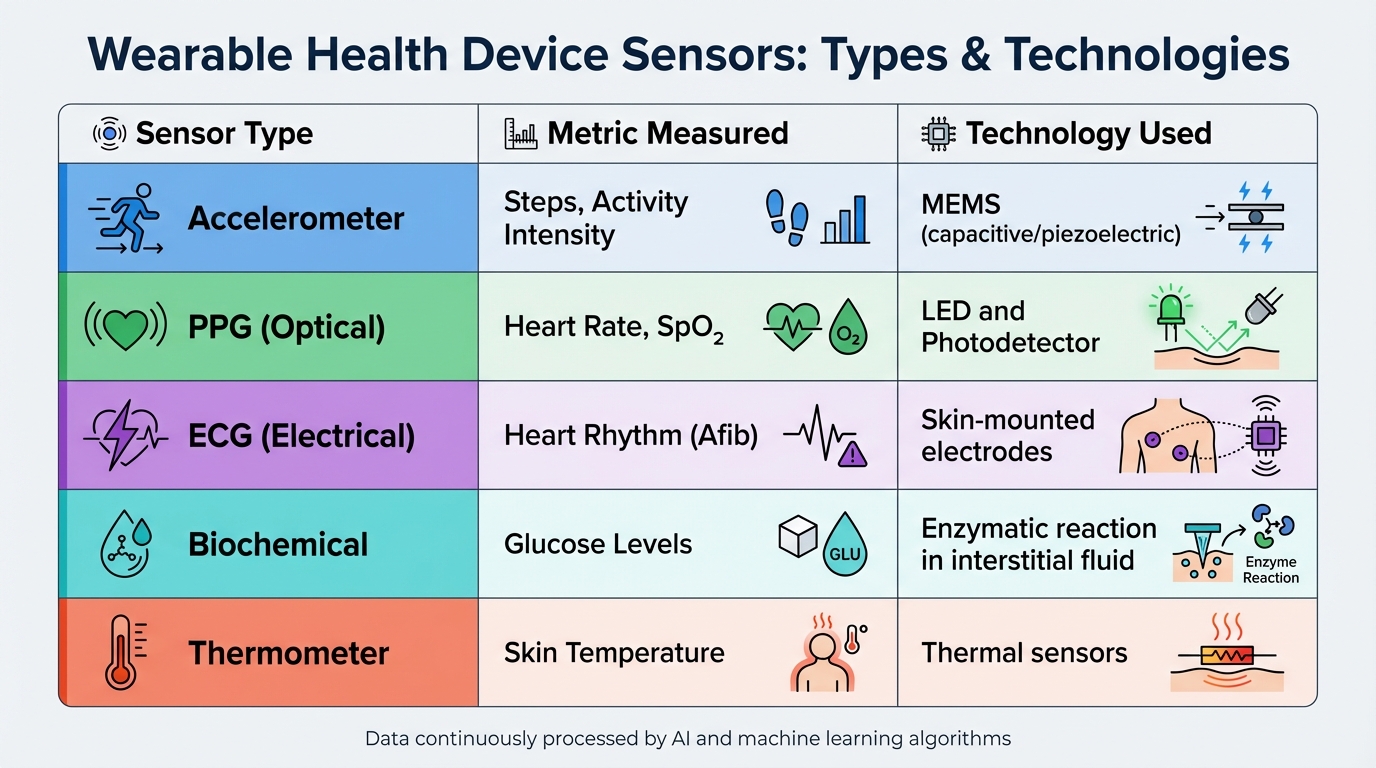
| Sensor Type | Metric | Technology Used |
|---|---|---|
| Accelerometer | Steps, Activity Intensity | MEMS (capacitive/piezoelectric) |
| PPG (Optical) | Heart Rate, SpO₂ | LED and Photodetector |
| ECG (Electrical) | Heart Rhythm (Afib) | Skin-mounted electrodes |
| Biochemical | Glucose Levels | Enzymatic reaction in interstitial fluid |
| Thermometer | Skin Temperature | Thermal sensors |
Each type of wearable device offers unique capabilities, making them versatile tools for monitoring and managing health.
What Health Conditions Can Wearable Devices Monitor?
Wearable devices have come a long way from just counting steps. These gadgets now tackle a variety of health concerns, from tracking heart rhythms to managing blood sugar levels. They’re becoming essential tools for managing chronic diseases and spotting health issues early.
Chronic Disease Management
Modern wearables are making strides in chronic disease care, especially for heart health. Devices equipped with ECG sensors can detect irregular heart rhythms, like atrial fibrillation, and keep tabs on blood pressure around the clock. Take the Aktiia Bracelet, for instance. At $265, it tracks systolic and diastolic blood pressure without needing a manual cuff. For diabetes management, continuous glucose monitors (CGMs) have become indispensable. In the 2017 DIAMOND trial, participants with Type 1 diabetes using the Dexcom G4 Platinum CGM achieved a 0.3% greater reduction in hemoglobin A1c levels over 24 weeks compared to those relying on standard care.
Heart failure patients also benefit from wearable technology. The 2018 TIM-HF 2 study, which included 1,571 participants, revealed that remote monitoring – using ECG and blood pressure tracking – significantly reduced unplanned cardiovascular hospitalizations and all-cause mortality compared to traditional care. For patients transitioning from hospital to home, devices like the BioButton deliver continuous vital sign monitoring, offering particular value for those with COPD or congestive heart failure.
But wearables aren’t just about heart health – they’re also tackling respiratory, sleep, and musculoskeletal challenges.
Respiratory and Sleep Monitoring
Wearable devices have expanded into respiratory and sleep health. They measure oxygen saturation (SpO₂) and respiratory rates, aiding in the management of conditions like COPD, asthma, and sleep apnea. For example, the Apple Watch Series 6 demonstrated a mean bias of just –0.23% for oxygen saturation when compared to medical-grade monitors. Meanwhile, devices like the Oura Ring Gen3 ($299) and Withings ScanWatch track SpO₂, heart rate variability, and sleep patterns, helping to spot breathing irregularities during sleep.
Although these devices are adept at identifying sleep-wake cycles, they often overestimate sleep efficiency – the percentage of time spent asleep while in bed. While polysomnography remains the gold standard for diagnosing sleep disorders, wearables offer the advantage of multi-night monitoring in your own home, capturing patterns that a single night in a sleep lab might miss.
Spine and Posture Health
Wearables are also carving out a niche in musculoskeletal health, particularly for spine care. With back pain costing the U.S. an estimated $60 billion annually, these devices are stepping in to help. Using inertial measurement units (IMUs) – which combine accelerometers, gyroscopes, and magnetometers – these wearables track spinal curvature, joint angles, and posture throughout the day. They provide real-time feedback through vibrations, sounds, or visual alerts, encouraging users to correct poor posture, such as a forward-leaning head or slouched shoulders.
Advanced sensors, like strain gauges and fiber-optic goniometers, go further by measuring lumbopelvic flexion and vertebral motion across multiple planes. On top of that, AI and machine learning analyze movement, gait, and standing time to predict pain levels and functional disabilities. In studies, machine learning models using wearable data accurately categorized pain intensity levels (mild, moderate, severe) 76.8% of the time. Additionally, stand time – a crucial metric for social and physical activity – increased significantly after spinal cord stimulation therapy.
"Wearable technologies… have the potential to revolutionize spine healthcare through their ability to collect data continuously and in any environment." – Ram Haddas, PhD, MBA
Key Benefits of Using Wearable Health Devices
Continuous Health Monitoring
Traditional healthcare often relies on isolated snapshots – a quick blood pressure check here, a heart rate reading there. But these spot-checks, typically capturing just four readings a day, leave significant gaps in data – missing about 96% of potential information. Wearable devices fill these gaps by recording 1,440 measurements daily, offering a detailed picture of your health. This constant stream of data can detect critical issues like sudden blood pressure spikes or irregular heart rhythms that routine check-ups might overlook.
This level of monitoring doesn’t just benefit patients – it also makes a financial impact. Hospitals save approximately $19,940 per bed each year, and this technology could potentially prevent up to 200,000 deaths annually. For individuals, it means fewer disruptions for medical visits and more confidence in their health management.
Early Detection and Preventive Care
The continuous data from wearables doesn’t just sit idle – it actively works to identify problems before they escalate. These devices excel at spotting early warning signs, allowing for timely interventions. For example, the LINK-HF study tracked 100 patients using a multisensor chest patch after hospitalization. The results? Machine learning algorithms flagged potential readmissions with 76–88% sensitivity and 85% specificity, providing alerts an average of 6.5 days before hospitalization.
Blood pressure monitoring also highlights the value of wearables. In a 2016 study involving 400 patients, those using a digital blood pressure cuff and app were more than twice as likely to achieve their target blood pressure compared to those receiving standard care – 71% versus 31%. Even for chronic pain sufferers, smartwatch data analyzing metrics like heart rate and step count accurately predicted pain intensity levels with 76.8% accuracy. These examples show how wearables shift healthcare from reactive to preventive.
Remote Monitoring and Personalized Feedback
Wearable devices don’t just detect issues – they actively support ongoing health management. By enabling remote patient monitoring, they provide personalized, real-time insights that help patients and healthcare providers make better decisions. Unlike traditional systems that rely on rigid thresholds, advanced wearables create individualized baselines, reducing unnecessary alerts and tailoring feedback to each person.
"For patients leaving the hospital, the wearable monitors can allow for peace of mind and earlier discharge because the individual continues to be monitored remotely." – CADTH
Remote monitoring also streamlines healthcare workflows. Automated data collection reduces errors in medical records, freeing up providers to spend more time on patient care. Meanwhile, patients benefit from actionable feedback – like vibration reminders to fix posture or alerts about elevated heart rates during exercise. This constant guidance empowers individuals to take charge of their health throughout the day.
sbb-itb-44aa802
What to Consider When Choosing a Wearable Health Device
Device Features and Capabilities
When picking a wearable health device, focus on features that suit your specific health needs. For managing chronic conditions like diabetes or heart disease, continuous monitoring is a must. Look for devices that can track data continuously for at least seven days to provide insights into daily patterns and long-term trends. If heart health is your priority, understand the difference between PPG sensors, which handle general heart rate monitoring, and ECG sensors, which are required to detect rhythm irregularities like atrial fibrillation. For instance, wrist-worn devices have shown a 0.97 diagnostic accuracy for atrial fibrillation.
Accuracy is another critical factor. Choose clinically validated devices that adhere to standards like COSMIN or AAMI/ESH/ISO for blood pressure monitoring. Be cautious, as some fitness trackers can miscalculate calories burned by over 20%, and certain pulse oximeters have been found to miss low blood oxygen levels more frequently in Black patients compared to white patients. For spine health, opt for smart apparel with tension fabrics that provide feedback to help you maintain proper posture, rather than devices that only offer passive support. Beyond the technical specs, consider comfort and whether the device integrates seamlessly with your smartphone.
Comfort, Compatibility, and Connectivity
Smartphone compatibility is a key consideration. For example, Apple Watches pair exclusively with iPhones, while Wear OS devices typically work with Android. Brands like Fitbit and Garmin, however, offer cross-platform compatibility. Before making a purchase, download the device’s app from the App Store or Google Play to confirm it works with your phone and operating system. It’s worth noting that in February 2025, the FDA issued a safety communication highlighting how smartphone OS updates or changes in settings can disrupt the functionality of compatible medical devices, such as insulin pumps and glucose monitors.
"In general, buying a smartwatch or fitness tracker that matches your phone brand can ensure seamless compatibility." – Consumer Reports
Check your phone’s notification settings to ensure you’ll receive critical alerts. Also, prioritize devices that are water-resistant and made from non-irritating materials for comfort during everyday use. A dependable battery life and overall durability are equally important, as discussed next.
Battery Life and Durability
Battery life plays a big role in the convenience of continuous monitoring. Look for devices with at least seven days of battery life to minimize the need for frequent charging. Keep in mind that features like GPS tracking and cellular connectivity can drain the battery faster – some devices last only a couple of days, while others can go beyond two weeks.
"Ideally greater than seven days for infrequent charging to reduce user burden; charging a device daily is least ideal." – Jessica K Lu, MEng, Centre for Healthy Longevity
Durability is just as important as battery performance. Choose a device that’s easy to clean and water-resistant to ensure it holds up over time. Stick to newer models from original manufacturers to benefit from ongoing firmware updates and software compatibility. Basic fitness trackers generally cost between $100 and $250, while advanced smartwatches with features like EKG and sleep apnea detection can cost $250 to $800 or more. Remember, a higher price doesn’t always mean better accuracy – focus on clinical validation and the features that align with your health goals.
The Role of AI and Machine Learning in Wearable Technology
AI-Driven Health Insights
AI takes the raw data collected by wearable sensors and turns it into detailed, personalized health information. Instead of relying on generic averages, machine learning creates a baseline tailored specifically to your body by analyzing your historical data. This is important because what’s normal for one person could indicate a problem for someone else. For example, an elevated blood pressure reading might be typical for one individual but concerning for another.
A study published in Nature (2019–2023) focused on 15 participants with chronic pain who used Apple Watch Series 3 devices. By tracking key health metrics, researchers used a Random Forest machine learning model to predict pain levels – mild, moderate, or severe – with an accuracy of 0.768 ± 0.012.
"Wearable biomarkers can be used to predict therapy outcomes in people with chronic pain, enabling continuous, real-time monitoring of patients during the use of implanted therapies." – Nature
Another breakthrough came from the Stanford University iPOP wearables study, published in Nature Medicine in May 2021. This research demonstrated how personalized machine learning models could predict lab results, such as hemoglobin levels and fasting glucose, by analyzing continuous heart rate and skin temperature data. The accuracy of these predictions improved significantly as the models incorporated more historical data from each participant.
These personalized insights lay the groundwork for wearable devices to identify potential health issues through anomaly detection.
Real-Time Anomaly Detection
AI-powered wearables take health monitoring to the next level by identifying potential problems before symptoms even appear. They achieve this by detecting deviations from your usual patterns. By combining physiological data (like heart rate) with behavioral data (such as activity levels), these devices can distinguish between expected variations and real health risks.
In August 2025, researchers from Sapienza University of Rome conducted a pilot study using the "AI on the Pulse" system with six elderly patients suffering from neurodegenerative conditions. Over three months, the system flagged 32 health anomalies, including hypertension episodes and irregular heart rate variability (HRV). A senior geriatrician confirmed these findings, with the system achieving a 93.75% true positive rate and outperforming 12 other methods by 22% in F1 score.
"By operating with non-invasive, lightweight devices like smartwatches, our system proves that high-quality health monitoring is possible without clinical-grade equipment." – Davide Gabrielli, Sapienza University of Rome
With wearable devices capturing over 250,000 bodily measurements daily for each user, AI has access to an enormous dataset. This allows it to spot subtle warning signs early, enhancing both general health monitoring and care for specific conditions like chronic diseases or spinal issues.
The ability to provide real-time alerts is only part of the story. Wearable devices are also designed to improve over time, thanks to continuous algorithm updates.
Continuous Algorithm Improvement
Wearable technology gets smarter the more you use it, as machine learning models continuously refine themselves based on the data they collect. The FDA has recognized this capability, stating that "one of the greatest benefits of AI/ML in software resides in its ability to learn from real-world use and experience, and its capability to improve its performance". To support this, the FDA has introduced "Predetermined Change Control Plans", which allow AI-driven medical devices to update post-market clearance while ensuring safety.
The Fitbit Heart Study, which included 455,699 participants, demonstrated the power of this approach. Using a PPG-based algorithm, the study achieved a 98.2% positive predictive value for detecting atrial fibrillation. This shows how algorithms trained on large datasets can deliver highly accurate, clinically relevant results.
Wearables are also moving toward edge intelligence, where AI processing happens directly on the device instead of in the cloud. This shift enables faster feedback, improved privacy, and consistent accuracy. Research further highlights that the longer you wear your device, the better it performs. Over time, it builds a more comprehensive understanding of your unique health patterns, making predictions increasingly precise.
Limitations and Challenges of Wearable Health Devices
Comfort and Usage Concerns
Wearable devices, when not properly fitted, can cause skin irritation and create motion artifacts that reduce the accuracy of the data they collect. Additionally, the constant notifications from these devices can overwhelm users, leading to what’s known as "alert fatigue." Instead of improving health, this can heighten anxiety. Some users even begin to doubt their own physical sensations, relying too heavily on device metrics. This over-dependence has been termed "wearables fatigue", with many users abandoning their devices within three to six months. A study tracking adult users of wristwatch-style biosensors showed that daily wear time dropped from an average of 13.3 hours to just 6.3 hours over a six-month period.
"The viability of wearable technology is not based on slick sensors or fashionable appearances alone. It is a function of the level of integration of the technology into the human lifestyle." – Guus de Hoog, Creative Director, Elitac Wearables
To address these challenges, Ochsner Health System implemented an innovative solution between 2015 and 2017. They introduced the "O-Bar", modeled after the Apple Genius Bar, where staff helped patients set up their devices. This approach eased the technical burden on clinicians by delegating it to a dedicated support team. The results were impressive: 71% of patients in their digital hypertension program achieved target blood pressure control within 90 days, compared to just 31% with standard care. However, these usability hurdles can still limit the effectiveness of wearables in managing chronic conditions, as they often lead to inconsistent data collection.
Data Privacy and Security
Beyond usability, wearables face serious challenges when it comes to data privacy and security. Most consumer devices fall outside the scope of HIPAA regulations, leaving sensitive health data vulnerable when stored in the cloud. This lack of protection means personal health information can often be shared with third parties without the stringent safeguards provided under HIPAA.
A notable case highlighting these concerns occurred in August 2025, when Whoop Inc. faced a proposed class action lawsuit (Lomeli v. Whoop Inc.) in the U.S. District Court for the Northern District of California. The plaintiff, Steven Lomeli, accused Whoop of embedding a third-party tracker, Segment, into its app to share sensitive health data – such as heart rate, sleep patterns, and reproductive health metrics – without user consent. The lawsuit seeks to represent a nationwide class under the Video Privacy Protection Act (VPPA) and the California Medical Information Act (CMIA).
The risks are not hypothetical. In 2021, a data breach exposed 61 million health records from Fitbit and Apple Watch users, including names, genders, ages, and locations. While 35% to 50% of users are open to sharing health data with researchers, this willingness hinges on transparency and giving users control over their information.
"HIPAA protects health data used by a covered entity (e.g., a provider or insurer). But when a consumer enters data into a health app or uses a wearable to track health metrics, their data isn’t subject to HIPAA." – Milberg Law Firm
Limited Validation and Performance Factors
Measurement accuracy is another major issue for wearable devices. The reliability of data varies depending on the metric being tracked. For example, most wearables use photoplethysmography (PPG) with green LED lights, which can be less accurate for individuals with darker skin tones, as melanin absorbs the light. In fact, these sensors can be up to 15% less accurate for people with darker skin. Pulse oximeters, specifically, are three times more likely to miss low blood oxygen levels in Black patients compared to white patients.
Energy expenditure metrics are particularly unreliable. Studies show that major brands can have errors exceeding 30% when estimating calories burned. A separate study of seven wrist-worn fitness trackers found calorie calculations to be off by more than 20%. While step counts and heart rate readings are generally more accurate, they can still be affected by factors like motion artifacts, skin thickness (linked to BMI), tattoos, freckles, and even certain medications like ADHD stimulants or beta-blockers.
Adding to the problem, many companies rush to release new features without thorough validation for clinical accuracy. Most wearables are "FDA Cleared" rather than "FDA Approved." This means devices are deemed "substantially equivalent" to existing products but are not always required to undergo rigorous clinical trials to prove their accuracy.
"The protection consumers assume they receive may be misguided so it is highly recommended that consumers do their own research before purchasing these wearable health devices." – National Center for Health Research
Conclusion
Wearable devices have come a long way, evolving from simple step counters to sophisticated tools powered by AI. These gadgets now track everything from heart rhythms to posture, offering an impressive level of insight. For example, continuous monitoring with wearables can provide up to 1,440 vital sign measurements in a single day, compared to just four manual checks.
That said, it’s important to remember that wearables are meant to complement professional medical care, not replace it. As Kaiser Permanente puts it:
"Wearables don’t replace the services you get at medical facilities… it’s a tool to use to add to the care you already get – not as a substitute for visiting a doctor".
However, these devices aren’t without their challenges. Issues like reduced sensor accuracy for people with darker skin tones and the lack of HIPAA protection for most consumer wearables remain significant concerns.
When choosing a wearable, consider these five factors: its ability to provide continuous monitoring, the device’s overall accuracy, ease of use (including battery life and comfort), availability, and cost. Also, ensure the device has FDA clearance and regularly review your smartphone settings to receive critical alerts.
The National Center for Health Research also advises caution:
"The protection consumers assume they receive may be misguided so it is highly recommended that consumers do their own research before purchasing these wearable health devices".
And don’t ignore your own instincts. If your wearable shows normal readings but you don’t feel well, trust your symptoms and consult a doctor.
Ultimately, wearable technology shines when paired with professional care. AI-driven insights and personalized feedback enhance their usefulness, but their true value lies in how they integrate with your clinical history, medical advice, and personal awareness. Wearables are a tool – not a standalone solution – and their success depends on realistic expectations and informed decisions.
FAQs
How do wearable health devices help manage chronic diseases?
Wearable health devices have become a game-changer in managing chronic diseases, thanks to their ability to provide real-time monitoring of vital signs and health metrics. These devices keep track of key indicators like heart rate, activity levels, and other symptoms, offering a continuous stream of data. This steady flow of information helps patients and healthcare providers spot potential issues early, paving the way for quicker, more tailored interventions. For example, some wearables can monitor pain levels or assess how well a treatment is working, delivering insights that can lead to improved care strategies.
Beyond monitoring, these devices encourage patients to stick to their treatment plans by offering tools for tracking progress and providing motivational feedback. They also excel in remote patient monitoring, cutting down the need for frequent in-person visits while ensuring steady oversight of conditions such as diabetes, cardiovascular diseases, or chronic pain. By giving patients the tools to actively participate in their care and supporting decisions with data, wearable technology has the potential to enhance both health outcomes and overall quality of life.
What factors should I consider to ensure a wearable health device is accurate?
To make sure a wearable health device delivers precise data, pay close attention to its reliability and whether it has undergone scientific validation. Look for evidence of clinical studies or professional health reviews that confirm its ability to measure key metrics like heart rate, steps, or sleep patterns accurately.
You should also evaluate the sensor quality and how effectively the device tracks data in various situations. Devices that perform consistently under different movement levels or environmental conditions tend to provide more dependable results. Checking user reviews and expert assessments can give you helpful feedback on the device’s accuracy and overall performance.
How do wearable health devices protect my personal data?
Wearable health devices keep your personal data safe by using encryption and secure communication protocols. These tools work together to protect your health information during transmission and storage, making it harder for anyone unauthorized to access or alter your data.
To add another layer of security, manufacturers include authentication protocols to verify user identity. They also roll out regular software updates to fix potential security gaps. On top of that, many devices meet strict regulatory standards aimed at safeguarding sensitive health information, ensuring you have more control and confidence in how your data is handled.

