Remote Patient Monitoring (RPM) has become a key part of healthcare in 2026, allowing doctors to track patients’ health data remotely using digital devices. This technology is transforming care for chronic conditions like diabetes, hypertension, and spine health while reducing hospital visits and costs. Here’s what you need to know:
- Adoption Growth: Over 50 million Americans now use RPM, supported by advancements in AI and wearable devices.
- Cost Impact: RPM has shown to cut hospitalizations by 87% and reduce deaths by 77%, saving billions in healthcare expenses.
- AI Integration: AI tools filter data, predict complications early, and improve accuracy of monitoring.
- Wearable Devices: Devices like smartwatches and under-the-mattress sensors track vital signs without disrupting daily life.
- Expanded Coverage: New billing codes in 2026 cover more conditions, including spine and musculoskeletal care.
- Patient Benefits: RPM minimizes clinic visits, improves convenience, and provides real-time health insights.
With the U.S. RPM market projected to double by 2030, this technology is reshaping healthcare delivery, making it more efficient and patient-focused.
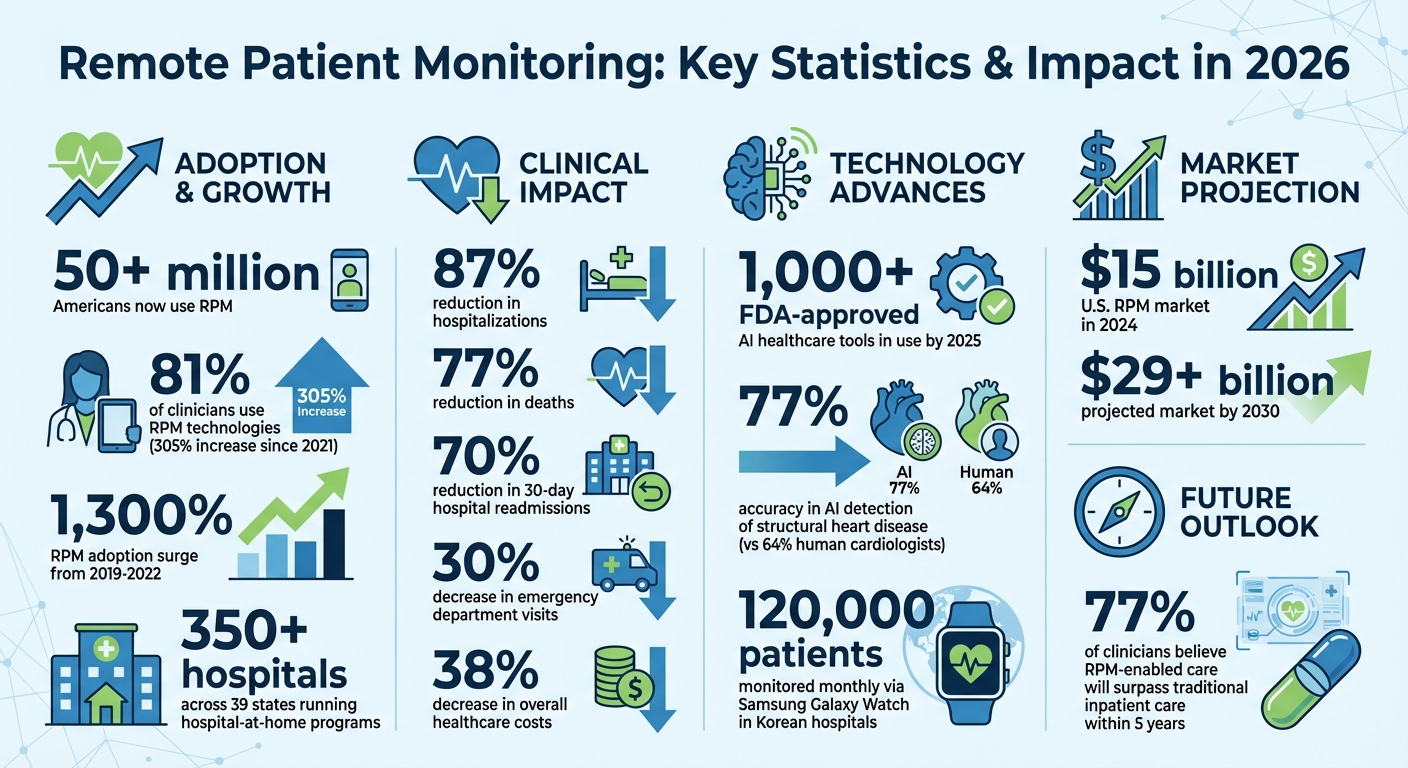
Remote Patient Monitoring Statistics and Impact in 2026
Wearables, remote patient monitoring & the future of chronic care management with Richard Milani, MD
RPM Technology Developments by 2026
The technology behind remote patient monitoring (RPM) has come a long way. By 2025, over 1,000 FDA-approved AI healthcare tools were already in use. These tools now provide real-time insights that were once unimaginable. Thanks to artificial intelligence, advanced sensors, and seamless data sharing, RPM systems have become an effective early warning system. They tackle three key challenges: improving measurement accuracy, enabling continuous tracking without burdening patients, and ensuring care teams have instant access to critical data. These advancements set the stage for the following discussions on AI, wearables, and data integration.
AI and Machine Learning in RPM
Artificial intelligence has become the driving force behind modern RPM systems. AI algorithms now filter out irrelevant data, ensuring only clinically significant information reaches healthcare providers. This reduces false alarms caused by sensor issues or patient movement, giving clinicians accurate readings they can trust.
One major leap is personalized baseline monitoring. Tools like "AI on the Pulse" use time-series models to learn each patient’s unique physiological patterns. Instead of relying on generic averages, these systems detect subtle changes in your normal patterns, identifying early warning signs that might otherwise go undetected.
"AI is truly revolutionizing remote patient monitoring: it enhances what can be measured and analyzed remotely, yields demonstrable improvements in care, and is reshaping healthcare delivery models." – Adrien Laurent, Author, IntuitionLabs
Predictive analytics is another game-changer. By analyzing trends over days or weeks – like weight changes, heart rate, or respiratory patterns – AI can predict complications, such as heart failure or hospital readmissions, days before symptoms appear. For instance, Columbia University’s "EchoNext" AI tool reviewed 85,000 ECGs and identified 3,400 undiagnosed cases of structural heart disease with 77% accuracy, outperforming human cardiologists at 64%.
AI also automates patient triage. Stable patients are flagged as "green lights", while concerning data triggers immediate alerts. This system allows providers to focus on the patients who need attention most, improving care efficiency and outcomes.
Advanced Wearable Devices
By 2026, wearable devices have become smarter, smaller, and more capable than ever. Devices like the BioIntelliSense BioSticker now track multiple vitals – such as skin temperature, respiratory rate, and even gait analysis – all from a single device. This gives clinicians a comprehensive view of a patient’s health without requiring multiple gadgets.
A standout advancement is cuffless blood pressure monitoring. Using optical sensors (PPG) and AI algorithms, wearables can now estimate blood pressure continuously, eliminating the need for bulky inflatable cuffs. In early 2025, Apple introduced a Watch-based AI system that alerts users to hypertension without a cuff. Similarly, Samsung’s Galaxy Watch now screens for Left Ventricular Systolic Dysfunction (LVSD) in over 100 Korean hospitals, monitoring approximately 120,000 patients monthly for early signs of heart failure.
Wearables have also become faster and more reliable thanks to edge computing. This allows devices to process data locally, detecting irregularities like heart arrhythmias or falls in real time, without waiting for cloud processing. Chest patches now stream high-quality cardiac data instantly.
Non-contact options, like "under-the-mattress" sensors, are also gaining traction. These devices monitor sleep, heart rate, and breathing without requiring patients to wear anything. This is particularly useful for elderly patients who may forget to charge or wear traditional devices. Such innovations not only simplify data collection but also enable timely interventions, as discussed further in the next section on data integration.
Data Integration and Interoperability
RPM platforms now integrate seamlessly with Electronic Health Records (EHRs) using HL7 and FHIR (Fast Healthcare Interoperability Resources) standards. This ensures that RPM data flows directly into a patient’s medical record, making it accessible to specialists, primary care providers, and emergency teams alike.
"Organizations need to prioritize EHR vendors that comply with the Fast Healthcare Interoperability Resources (FHIR) standard, which helps ensure that patient data is consistently shared across systems using various forms of exchange protocols." – Margaret Lindquist, Content Strategist, Oracle Health
Automated data flow has reduced manual errors and administrative burdens. Devices now operate "always-on", sending measurements directly to EHRs without patient involvement. Cloud platforms handle data from various Internet of Medical Things (IoMT) devices, process it through AI, and present actionable insights via clinician dashboards. This streamlined process eliminates the need for providers to juggle multiple systems, cutting down on errors and reducing "data noise".
Top RPM Devices for Chronic Disease and Spine Health
By 2026, remote patient monitoring (RPM) devices have evolved into highly reliable tools, providing continuous and accurate health data. Take the Apple Watch, for example – it now uses AI to detect conditions like atrial fibrillation, hypertension, and even early signs of heart failure.
But RPM technology isn’t just about heart health anymore. It’s expanded to address a variety of chronic conditions. For diabetes, devices like Abbott’s Libre Rio and Lingo continuous glucose monitors (CGMs) have become game changers. These over-the-counter monitors cater to the 24.5 million Americans with type 2 diabetes who don’t use insulin. They provide real-time glucose readings, eliminating the need for finger-stick tests entirely. Similarly, connected blood pressure cuffs, paired with smartphone apps, have shown impressive results – 84% of users with Stage II hypertension maintained control over their blood pressure for three years.
Spine health has seen remarkable advancements as well. Inertial measurement unit (IMU) sensors now monitor cervical spine range of motion and posture in everyday settings. For example, the BAIOBIT 1.8 platform, when placed on the external occipital protuberance, has demonstrated outstanding reliability (ICC > 0.90) in tracking movements like flexion-extension, lateral bending, and axial rotation. These wearable sensors excel at capturing data during real-world activities, offering insights that go beyond the clinical environment.
On top of these specialized tools, multi-parameter patches and under-the-mattress sensors now provide all-in-one monitoring of vital signs, simplifying patient care.
With such a wide array of RPM devices available, people with different health needs can easily integrate advanced monitoring into their daily routines.
Chronic Conditions Managed with RPM
Remote patient monitoring (RPM) has reshaped how chronic diseases are managed by giving healthcare providers access to continuous streams of patient data. This constant flow of information allows clinicians to move away from the traditional "wait and see" approach of periodic office visits. Instead, they can now act proactively, addressing potential problems before they escalate.
The benefits are especially clear for high-risk patients. Take, for example, a 2021 study conducted in Cleveland, Ohio, which tracked COVID-19 patients after hospital discharge. Patients monitored remotely saw 87% fewer hospitalizations and 77% fewer deaths compared to those without RPM. These statistics highlight how real-time data and timely interventions can prevent emergencies. With this foundation, let’s explore how RPM is revolutionizing care for diabetes, hypertension, and spine health.
Diabetes Management
For people with diabetes, RPM has been a game changer. Continuous glucose monitors (CGMs) have largely replaced the need for frequent finger-stick tests. These devices provide real-time glucose readings, empowering patients to make immediate adjustments to their diet or medications. The results speak for themselves: 70% of high-risk diabetic patients using RPM devices successfully lowered their A1C levels. This is significant because lower A1C levels reduce the risk of long-term complications like heart disease, kidney issues, and nerve damage.
Hypertension Monitoring
RPM is also making strides in managing high blood pressure. Traditional in-office blood pressure readings often fail to capture the full picture, missing cases of masked or stress-induced hypertension. With connected blood pressure cuffs, patients can now monitor their blood pressure from the comfort of their homes, providing clinicians with more accurate and consistent data.
At Mass General Brigham‘s Accelerator for Clinical Transformation in 2023, RPM tools allowed pharmacists to adjust medications remotely based on this data. The result? Participants achieved better control of both blood pressure and cholesterol levels. Other studies have echoed these findings, showing that ongoing monitoring through connected devices leads to sustained improvements in blood pressure management.
Spine Health and Posture Correction
RPM is also making waves in musculoskeletal care, particularly in spine health and posture correction. Wearable sensors are now being used to monitor spine alignment and posture in ways that traditional clinical settings simply can’t. These devices track recovery after surgery, measure movement patterns, and alert clinicians to any potential complications. This means patients can recover safely at home while their care teams remain informed about their progress.
Beyond recovery, RPM supports long-term musculoskeletal health through Remote Therapeutic Monitoring (RTM). RTM programs track therapy adherence and provide feedback to improve posture and movement habits during everyday activities. This ensures patients not only recover but also maintain healthier movement patterns over time.
sbb-itb-44aa802
How to Implement RPM Programs
Starting a remote patient monitoring (RPM) program requires careful planning and well-defined workflows. The first step? Build a team that brings together clinical staff, IT experts, and administrative leaders. This group should focus on identifying the specific challenges your practice faces – whether it’s reducing readmissions, improving medication adherence, or addressing gaps in managing chronic conditions. Once these issues are clear, set measurable goals to tackle them.
"You have to intimately understand and appreciate how a process works from the perspective of the patient, providers and caregivers and each operational stakeholder before you can improve or replace it."
– Omid Toloui, Vice President of Digital Health, CareMore
After setting your goals, create a workflow that assigns clear responsibilities. Who will recruit and onboard patients? Who will monitor data during and after hours? And who will handle tech support if a device stops working? With nearly 90% of healthcare providers already investing in or evaluating RPM technologies, this structured preparation is key to ensuring smooth patient onboarding and system integration.
Patient Onboarding and Education
Start by identifying eligible patients – those with chronic conditions like diabetes, hypertension, or spine issues – and obtaining their documented consent. It’s important to ensure patients fully understand what RPM entails. As Neal Sikka, Professor of Emergency Medicine at George Washington University, points out:
"Many patients do not know what to expect. You have to provide a clear expectation that while these data are going to come to us right away, a clinician will react to a trend rather than each data point."
Education is crucial here. Patients need to know how to distinguish between an out-of-range reading and an actual medical emergency. For instance, if their blood pressure spikes or glucose levels drop dangerously low, they should call 911 immediately. During the first couple of weeks, provide hands-on training to help patients pair devices, transmit data, and navigate patient portals or mobile apps. For those without reliable internet or digital skills, cellular-enabled devices can simplify the process by eliminating the need for Wi-Fi or smartphones. Once patients are fully informed and comfortable, the focus shifts to setting up and integrating their monitoring devices.
Device Setup and Integration
Choosing the right devices is critical to the success of your RPM program. Prioritize FDA-cleared devices that support reliable data transmission via cellular, Bluetooth, or Wi-Fi. Cellular-enabled devices are particularly helpful for older adults or rural patients who may lack stable internet or smartphones. After selecting devices, set up patient profiles and integrate them with your EHR system.
Next comes calibration, typically during weeks two and three. This phase ensures accurate data transmission and resolves any connectivity issues. Set clinical thresholds for automated alerts tailored to each patient’s specific needs. For example, a patient with stable hypertension might have different alert settings than someone with more fluctuating readings. As Colton Hood, Assistant Professor of Emergency Medicine at George Washington University, explains:
"Remote monitoring almost needs to be personalized per patient and per disease. There are some conditions in which you may tolerate slightly out-of-range readings, but someone else may look at that data without being familiar with that program or the patient and may not have the same assessment."
Proper device setup is essential for collecting reliable data that supports timely clinical decisions. Keep in mind, Medicare requires at least 16 days of data transmission within a 30-day period to qualify for reimbursement under CPT code 99454.
Monitoring and Clinical Workflow Integration
Use a centralized provider dashboard to track high-risk patients and review incoming data daily. Many modern RPM platforms now include AI and machine learning tools to flag anomalies, detect medication side effects, and recommend care plan adjustments.
Assign dedicated staff to monitor dashboards and provide timely feedback to patients, which not only enhances engagement but also ensures prompt follow-ups. Be sure to document all clinical interventions and the time spent reviewing data – this is essential for billing under CPT codes 99457 (for the first 20 minutes of clinical staff time per month) and 99458 (for each additional 20 minutes). Automating alerts and streamlining documentation can also help reduce administrative burdens. Finally, review your RPM program every three to six months to evaluate patient outcomes, adjust care plans, and maintain engagement. This ongoing evaluation ensures RPM remains a proactive tool for managing chronic conditions.
| Implementation Phase | Timeframe | Key Activities |
|---|---|---|
| Assessment & Eligibility | Week 1 | Identify conditions, verify insurance, obtain patient consent. |
| Device Selection & Enrollment | Week 1–2 | Order FDA-cleared devices, set up patient profiles, train patients. |
| Calibration | Weeks 2–3 | Confirm accurate pairing, resolve connectivity issues, set thresholds. |
| Active Monitoring | Ongoing | Daily data review, trigger alerts, document interventions. |
| Reporting & Billing | Monthly | Confirm 16-day data, compile reports, and submit CPT claims. |
| Reassessment | Every 3–6 Months | Review patient status, adjust care plans, confirm engagement. |
2026 CMS Billing and Reimbursement for RPM
The Centers for Medicare & Medicaid Services (CMS) has expanded reimbursement options for both short-term and long-term Remote Patient Monitoring (RPM). Providers can now bill for shorter interactions, such as brief data transmissions or management sessions. New codes like CPT 99445 (for 2–15 days of monitoring) and CPT 99470 (for 10–19 minutes of treatment management) allow billing for services like post-discharge recovery or medication adjustments. This ensures that even advanced RPM data collection is aligned with reimbursement policies.
Daniel Tashnek, CEO of Prevounce Health, highlights the significance of these changes:
"Clinicians can now bill for fewer monthly vital readings and shorter management time. For patients, this means RPM programs can finally match clinical reality."
Providers must choose the appropriate codes based on actual data transmission and clinical time. For treatment management, at least one live, interactive communication with the patient or caregiver is required each month – text messages or asynchronous chats do not meet this standard. These updates are designed to integrate smoothly into clinical workflows.
CPT Codes for RPM
The 2026 billing framework includes both familiar and new codes to accommodate a range of monitoring durations and clinical time commitments. For instance, CPT 99453 now requires a minimum of 2 days of monitoring data for reimbursement, estimated at $22. Device supply codes include CPT 99445 for short-term monitoring (2–15 days) and CPT 99454 for standard monitoring (16–30 days), both reimbursed at around $47. Treatment management codes have also been updated: CPT 99470 reimburses approximately $26 for 10–19 minutes of clinical staff time, while CPT 99457 offers $52 for 20 minutes. For extended care, CPT 99458 provides $41 for each additional 20 minutes.
| CPT Code | Service Description | Data/Time Requirement | 2026 Est. Reimbursement |
|---|---|---|---|
| 99453 | Initial setup and patient education | Minimum 2 days of monitoring | ~$22 |
| 99445 | Device supply (short-term) | 2–15 days in a 30-day period | ~$47 |
| 99454 | Device supply (standard) | 16–30 days in a 30-day period | ~$47 |
| 99470 | Treatment management | First 10–19 minutes per month | ~$26 |
| 99457 | Treatment management | First 20 minutes per month | ~$52 |
| 99458 | Additional management | Each additional 20 minutes | ~$41 |
CMS now uses Outpatient Prospective Payment System (OPPS) data to standardize device reimbursements, ensuring that costs for software, cloud storage, and cybersecurity are accurately reflected.
Billing Workflow Optimization
To streamline billing under the updated CPT codes, consider the following steps:
- Track Data Transmission: Ensure documentation workflows accurately record the number of days patients transmit data. Use CPT 99445 for 2–15 days and CPT 99454 for 16–30 days. Many RPM platforms can automatically flag when these thresholds are reached.
- Document Live Interactions: For management billing, record every live interaction with patients, whether via phone or video. These interactions, combined with activities like data review, care plan adjustments, and intervention documentation, form the basis for management codes. Use CPT 99470 for 10–19 minutes of routine check-ins and CPT 99457 for 20-minute sessions involving more complex care. For high-risk patients, CPT 99458 covers additional 20-minute increments.
- Verify Device Compliance: Ensure all devices meet the FDA’s definition of a medical device and automatically upload physiologic data. Self-reported data from patients does not qualify for RPM billing.
- Justify Medical Necessity: Clearly document the medical necessity for RPM enrollment, specifying the acute or chronic condition being managed and the corresponding treatment plan. CMS has increased audit scrutiny following a 2024 OIG report on billing inconsistencies, so thorough documentation is critical.
These updates not only simplify the billing process but also align RPM programs more closely with clinical needs and regulatory requirements.
AIH LLC: Advanced Remote Patient Monitoring Solutions
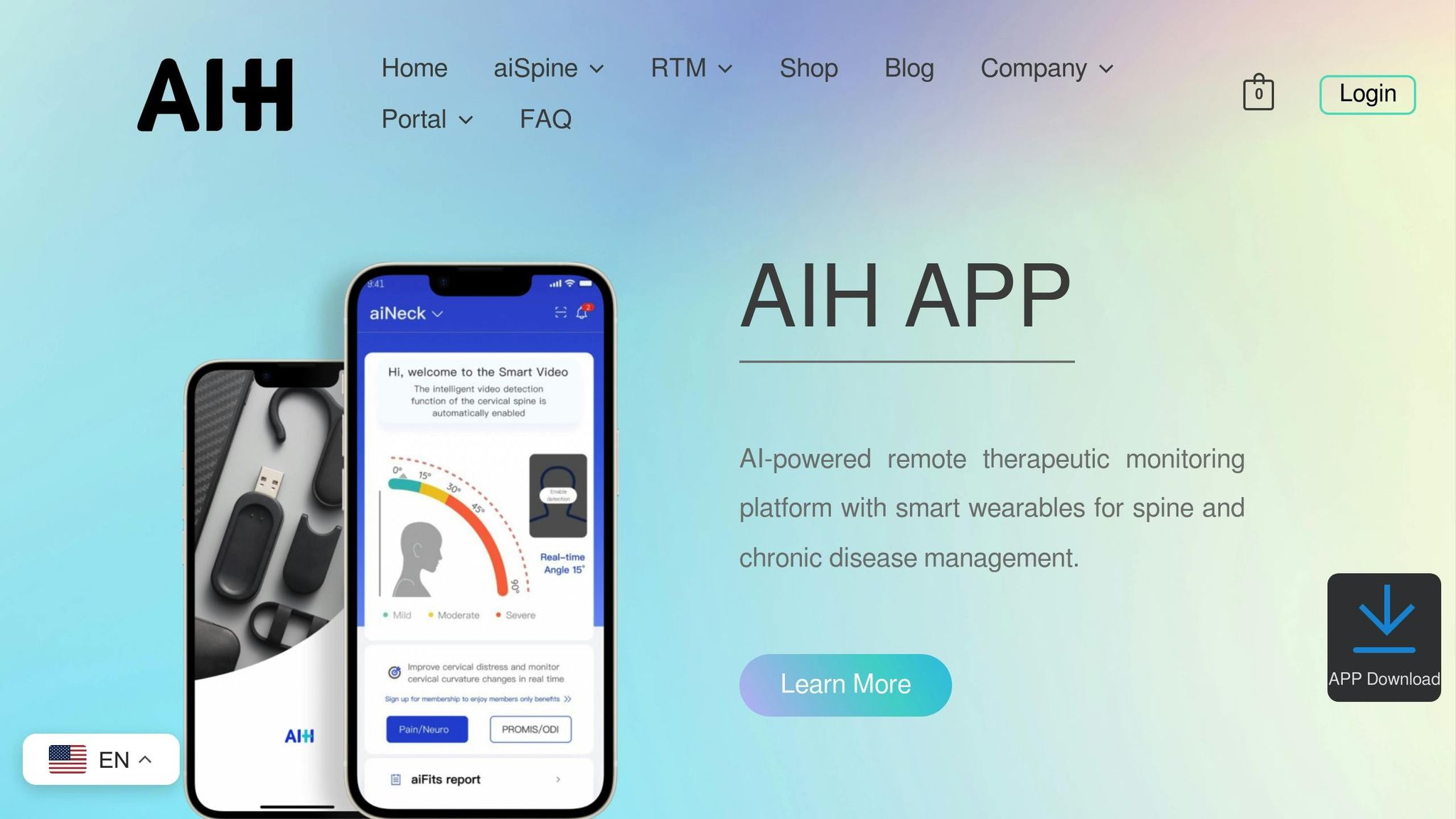
AIH LLC has taken remote patient monitoring (RPM) to the next level with its AI-powered wearable devices designed for spine health and chronic disease management. Their product lineup includes the aiSpine posture monitoring device, the aiRing vital signs tracking ring, and the soon-to-launch aiNeuro, which focuses on stroke risk assessment and posture correction. Each device works seamlessly with the AIH Health App, providing real-time tracking and tailored health insights.
The aiSpine continuously monitors spinal posture, sending instant vibration alerts when poor posture is detected. Meanwhile, the aiRing measures key health metrics like heart rate, oxygen saturation, and activity levels. Both devices automatically transmit data via Bluetooth 4.0, meeting FDA requirements and CMS reimbursement standards. These features are further amplified by their smooth integration with the AIH Health App.
AIH Health App Integration
The AIH Health App serves as the hub where data from all AIH devices comes together to form a detailed health profile. By analyzing sensor data, the app identifies trends and provides personalized recommendations, such as therapy adherence strategies and insights into patient-reported outcomes for spine health. The app transforms raw data into actionable insights, ensuring clinicians can easily integrate this information into their existing workflows.
FDA Compliance and Physician Training
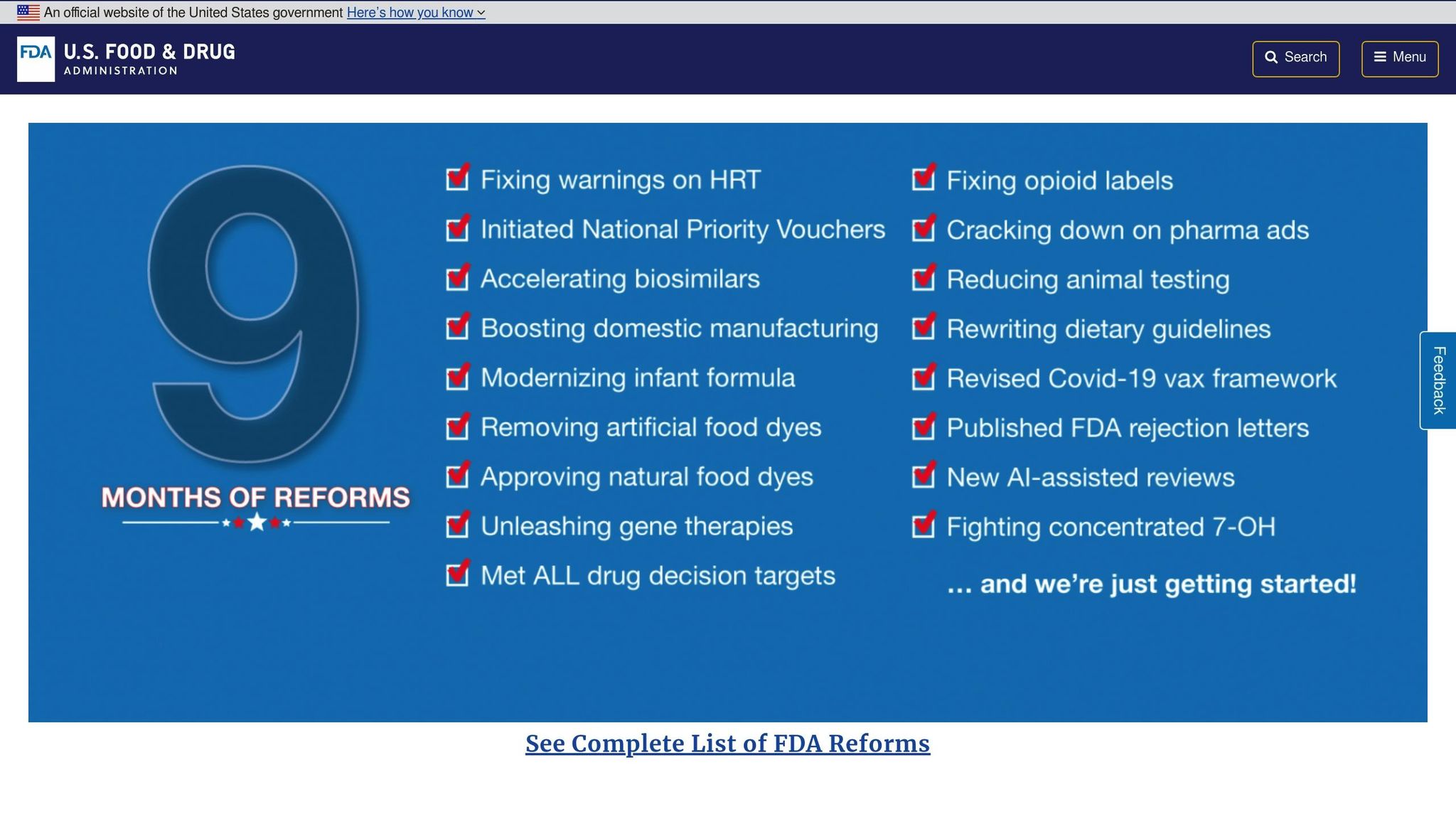
AIH LLC goes beyond just offering high-tech devices – it also supports healthcare providers every step of the way. The company ensures its devices meet rigorous FDA verification standards for accurate measurements and effective clinical use. Additionally, the devices comply with 2026 CMS requirements for automatic data transmission.
To help healthcare teams maximize the benefits of RPM, AIH LLC provides comprehensive physician training programs. These programs cover everything from onboarding patients and responding to device alerts to incorporating remote monitoring data into clinical decisions. Training also includes guidance on proper documentation for billing under RPM codes (CPT 99453–99458) and RTM codes (CPT 98975–98981) for musculoskeletal health monitoring. On top of this, AIH LLC places a strong emphasis on data security, using HIPAA-compliant protocols with end-to-end encryption to protect patient information both in transit and at rest.
Conclusion
By 2026, Remote Patient Monitoring (RPM) has transformed healthcare from a reactive, episodic system into one focused on continuous, proactive care. With 81% of clinicians now using RPM technologies – a staggering 305% increase since 2021 – its adoption continues to grow rapidly. The impact is undeniable: emergency department visits have dropped by as much as 30%, while case studies reveal a 70% reduction in 30-day hospital readmissions and a 38% decrease in overall healthcare costs. This momentum has also fueled advancements in AI-powered analytics and wearable technology.
The combination of AI analytics with sophisticated wearable devices has made early detection of health issues more accessible than ever. Currently, over 350 hospitals across 39 states are running CMS-waived hospital-at-home programs, which have been shown to reduce both mortality rates and costs. Adrien Laurent of Intuition Labs highlights this shift:
"RPM adoption from 2019 to 2022 surged ~1,300% in the U.S., a reflection of how quickly virtual care has been embraced in both chronic and acute settings".
Amid these advancements, AIH LLC is at the forefront, offering specialized solutions for spine health and chronic disease management. Their innovative products – aiSpine, aiRing, and the soon-to-be-released aiNeuro – provide real-time monitoring with automatic data transmission, meeting FDA verification standards and aligning with 2026 CMS reimbursement requirements. These devices, paired with the AIH Health App, deliver personalized insights and support healthcare providers with comprehensive training programs, enabling measurable improvements in patient outcomes.
Looking ahead, 77% of clinicians believe RPM-enabled care will surpass traditional inpatient care within the next five years. With the U.S. RPM market expected to grow from $15 billion in 2024 to over $29 billion by 2030, the role of RPM in managing chronic conditions, lowering healthcare costs, and improving quality of life is only set to expand. The future of healthcare is no longer confined to hospital walls – it’s being reshaped by intelligent monitoring systems that empower patients and providers alike.
FAQs
How does AI improve remote patient monitoring in 2026?
AI is reshaping remote patient monitoring (RPM) in 2026, turning raw health data from wearables and sensors into meaningful insights. Using advanced machine learning, these systems analyze vital signs, activity levels, and subtle physiological changes, delivering real-time alerts that help healthcare providers spot potential problems before symptoms even surface. By filtering out irrelevant data and emphasizing critical trends, these tools allow clinicians to focus their attention where it’s needed most.
AI also takes personalized care to the next level by understanding each patient’s unique health patterns. Predictive analytics can suggest timely interventions – like adjusting medications or recommending specific exercises – to improve patient outcomes and potentially cut down on hospital visits. With the integration of edge computing and secure cloud analytics, AI-powered RPM systems are not only efficient but also scalable, making them a powerful tool for managing chronic conditions and spine health across the U.S.
What are the main benefits of wearable devices for managing chronic conditions?
Wearable devices are transforming how healthcare professionals access real-time health data like heart rate, blood pressure, glucose levels, and activity metrics – all without requiring patients to step into a clinic. This kind of continuous monitoring makes it possible to catch potential health issues early, paving the way for timely interventions that can help prevent complications and reduce the need for emergency care.
By automatically collecting and transmitting health data, wearables also play a role in cutting down hospitalizations and readmissions. Fewer hospital visits mean not only cost savings but also an improved quality of life for patients. On top of that, these devices encourage patients to take charge of their own health, helping them stick to treatment plans and make adjustments tailored to their unique needs.
Thanks to their ability to deliver ongoing insights, support early intervention, and boost patient involvement, wearable devices are becoming an essential part of managing chronic diseases effectively in 2026.
How will the new 2026 billing codes affect reimbursement for remote patient monitoring?
The 2026 Medicare Physician Fee Schedule introduces updated CPT codes, making it simpler for healthcare providers to receive reimbursement for remote patient monitoring (RPM). For instance, CPT 99445 now allows billing for short-term monitoring – covering 2 to 15 days of data within a 30-day period, which was previously excluded. Meanwhile, CPT 99454 refines billing for device supply, addressing data transmission over 16 to 30 days. Additionally, CPT 99470 offers reimbursement for up to 10 minutes of provider-led care coordination each month.
These updates bring greater flexibility to RPM services by accommodating shorter monitoring durations, covering device-related costs, and recognizing the time providers spend on clinical management. The changes not only encourage wider use of RPM but also help providers establish more consistent revenue streams while enhancing their ability to deliver connected care.

